Giving Blood is an Essential Service
“A donation from just one person could save up to three lives” – these words are stated on The UWI Blood Donor Foundation’s (UWIBDF) website and have been repeated in blood donor campaigns globally. Yet there is a lack of voluntary blood donors in Trinidad and Tobago. How could that be?
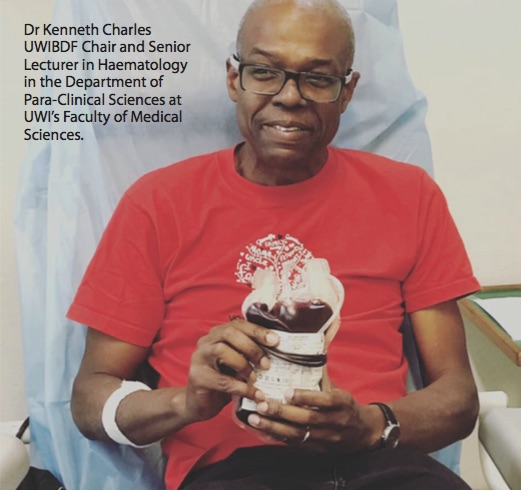
Blood is vital to life and a constant supply is necessary for patients such as pregnant women, those undergoing cancer treatment, persons with inherited blood disorders, and so many others. According to UWIBDF Chair Dr Kenneth Charles, Senior Lecturer in Haematology in the Department of Para- Clinical Sciences at UWI’s Faculty of Medical Sciences (FMS), the number of blood units collected annually has plateaued and further decreased since stay-at-home measures were implemented in Trinidad and Tobago.
UWIBDF and the Trinidad and Tobago Ministry of Health are collaborating to encourage people to voluntarily give and continue doing so during COVID-19. Last month, UWIBDF hosted its 16th Voluntary Blood Drive. UWIToday sat down (virtually) with Dr Charles to discuss the foundation’s role in increasing voluntary blood donation awareness, misconceptions surrounding donating, and why ensuring regular, safe access to blood donations should be our first priority.
The first aim is to promote awareness of voluntary non-remunerated blood donation in the university and the community. This has not changed.
Voluntary non-remunerated donors (VNRD) donate blood voluntarily, without pressure from the healthcare system, patients or relatives for nothing that could be considered payment in cash or kind. Currently, blood is collected from family replacement donors at hospital-based donation centres where close friends and family donate blood to be claimed for a named beneficiary. If not enough people donate, the beneficiary will not receive the quantity of blood they need. Voluntary non- remunerated blood donation is a safer alternative that ensures blood is collected and available to treat anyone in need (for example, persons needing monthly transfusions or emergency transfusions due to road accidents).
In FMS, students learn about it through lectures, practicums and research projects. Research findings are shared regionally and internationally. UWIBDF also conducts school visits and invites secondary school students to the World Blood Donor Day Symposium.
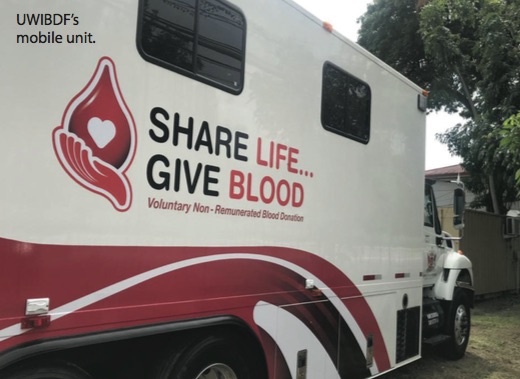
Since March 2015, UWIBDF in collaboration with the North Central Regional Health Authority has been hosting a blood drive which takes place three times a year. We consistently collect over 100 units of blood at each drive and add them to the national blood supply. Last month, we held our 16th Voluntary Blood Drive at the blood bank and using a mobile unit to accommodate more donors and maintain the social distance guidelines. We collected 67 units, which is a great effort.
National pride, altruism, a desire to help others, and taking up the challenge of fixing the blood shortage problem in this country. Overall, UWIBDF has VNRDs from the student body and the public who are motivated by these reasons.
Dr Waveney Charles was the first trained haematologist to practise in this country and single-handedly laid the foundation for haematology and blood banking services. Her work in developing a space for young persons with inherited blood disorders and their families will be a lasting legacy. She doggedly developed a national blood transfusion service which did not exist before 1986, within the constraints of the regulatory systems. Dr Waveney Charles personally trained most of the laboratory technologists who became the core of blood banking operations in the country. We can all learn about the power of listening to the needs of others from her, and how to identify solutions and implement them selflessly.
Our experience with UWIBDF in the last five years has taught us several things about how people come around to donating:
I would like to see the blood donation system changed to one that is 100 per cent reliant on VNRDs using public education and changes in the legal and regulatory pathways to facilitate voluntary non-remunerated blood donation. That means continued investment in our young people as the agents of this change. We would increase the amount of blood collected annually and make the supply safer and equally available. It could happen if the UWIBDF model is applied nationally.
If you are a healthy person of suitable weight, and age, you can register to become a donor on the UWBDF website. You can also encourage others to donate voluntarily through the Ministry of Health Blood Bank Services. It is a great time of national need, please do your part.
For more about The UWI Blood Donor Foundation, please visit http://uwiblood.com/ or their Facebook Page https://www.facebook.com/UWIBlood.
We already have a voluntary non-remunerated system.
Fact: More than 80 per cent of donated blood comes from replacement donors and most of the rest from persons who could reclaim their donations (they can donate blood for no specific person but then claim their blood for a named beneficiary at a later date).
Once blood is tested in the lab it is safe.
Fact: There is a window period before tests for infections become positive. Safety relies on truthfulness at the blood donation interview. This is why VNRDs are safest.
Persons could get infections from donating blood.
Fact: There is no risk of acquiring an infection from donating blood since sterile equipment is used and not reused. Sterile techniques as defined by international (Pan American Health Organisation) standards are used for collecting blood from donors.
You can get COVID-19 from donating blood.
Fact: COVID-19 is not spread through blood donation or transfusion.
Donated blood is stored for a long time.
Fact: Once collected, blood is separated into red cells which last about a month, platelets which last five days and plasma which is frozen for a year. Red cells are the most commonly used component so a steady flow of donations is required.