Surveys show cancer and glaucoma patients willing to use the natural remedy for treatment, but lacking knowledge of the plant and its side effects
Cancer is the second leading cause of death worldwide, with almost 2,000 deaths in Trinidad and Tobago in 2018. Glaucoma is the leading cause of blindness worldwide, with the Caribbean region having the highest prevalence globally.
Many patients in Trinidad and Tobago use “natural” remedies, including marijuana, to treat cancer and glaucoma. Marijuana is believed to alleviate cancer pain, chemotherapy- induced nausea and vomiting, as well as reduce intraocular (inside of the eye) pressure in glaucoma. Several cannabinoids in marijuana, such as THC (tetrahydrocannabinol) and CBD (cannabidiol), are responsible for its psychoactive properties and proposed medicinal effects.
In June and July 2019, a team of students from the Pharmacology Unit conducted two surveys on cancer and glaucoma patients related to the use of marijuana. At that time, there were legislative overtures in Trinidad and Tobago to decriminalise marijuana for medicinal, recreational and religious use. Therefore, we sought to determine among these patients:
These studies were approved by The UWI Campus Ethics Committee and the respective Regional Health Authorities Ethics Committees. Patients were asked to sign their informed consent before agreeing to participate.

The first survey consisted of 194 cancer patients at the Oncology Unit at the St James Medical Complex. Almost three-quarters of the cancer patients were female, with an average age of about 60 years old. Breast cancer (80 of 142 women) and prostate cancer (22 of 52 men) were the most common cancers, and about half of the patients were at either Stage III or IV. Most patients had already undergone surgery, chemotherapy and radiation therapy and were satisfied with conventional treatment. However, almost 80 percent reported having experienced side effects with conventional treatments.
In these patients, knowledge about marijuana was generally low with an average score of less than three out of 10. Few patients were able to identify one or more cannabinoids found in marijuana or its medicinal use. However, many patients recognised that marijuana could cause paranoia, hallucinations and memory impairment.
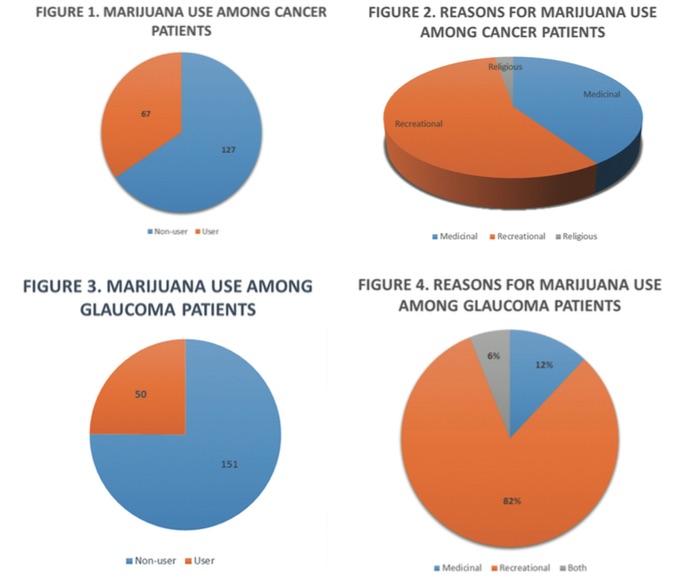
About one-third of cancer patients reported previous marijuana use for recreational, medicinal or religious purposes (Figures 1 & 2). Interestingly, about two-thirds of marijuana users did so for recreation. Significantly, marijuana use among this group was most prevalent among those who were male, of African descent, and experiencing side effects to conventional anticancer treatments.
Marijuana is believed to alleviate cancer pain, chemotherapy-induced nausea and vomiting, as well as reduce intraocular (inside of the eye) pressure in glaucoma.
Cancer patients who used marijuana for anxiety, insomnia, nausea and pain believed that it was very effective, that these benefits outweighed the risks, and that it was not addictive. Almost 90 percent of cancer patients indicated that they would use marijuana to treat their condition should it become legally available.
In the second survey, 201 glaucoma patients were recruited, with almost equal numbers of men and women with the average age of about 69 years old. Most patients were diagnosed with glaucoma for about eight years and were mostly satisfied with their medical treatment. Only a small number of patients reported having side effects related to their glaucoma medications.
About one-quarter of glaucoma patients reported previous use of marijuana (Figure 3). Being male, African descent and supporting decriminalisation were significant predictors of marijuana use. As with cancer patients, most marijuana users (over 80 per cent) did so for recreational purposes (Figure 4). Patients using marijuana for medicinal purposes such as asthma, arthritis and improvement of mood reported that it was very effective, and in some cases more effective than conventional medicines.
Like cancer patients, glaucoma patients had poor knowledge of marijuana, with over 70 per cent not being able to identify more than one medicinal use or side effect of marijuana. Despite poor knowledge, almost 80 percent of glaucoma patients stated that they would use marijuana medicinally as they believed that it would treat, cure or improve their glaucoma. However, there were no associations among demographic characteristics, treatment history, previous use of marijuana, and desire to use medical marijuana. Patients who were unwilling to use marijuana cited its side effects and stigma as barriers.
Additionally, ten ophthalmologists (with average of 12 years in clinical practice) were interviewed. These specialist doctors felt underprepared to advise patients on the medicinal use of marijuana and highlighted the need for more robust clinical evidence to inform their decisions.
They were concerned that public education was inadequate, and that increased accessibility following decriminalisation would escalate the potential for recreational use and drug abuse. The general consensus was that tight regulation of medical marijuana should be instituted to include patients’ substance abuse and social history, in addition to controlled dispensing by licensed healthcare professionals or pharmacies.
From these surveys, we found that significant numbers of cancer and glaucoma patients had a history of marijuana use, and most did so for recreational purposes. Despite having little knowledge, most patients were willing to use marijuana in the environment of decriminalisation.
There is an urgent need to address the impending increased use of marijuana among these and other subsets of patients in an environment of decriminalisation. A policy framework must be established to guide the use of medical marijuana and its derivatives in the clinical setting. Additionally, an immediate educational drive is warranted to fill the significant gaps in knowledge in both patients and physicians.
The surveys were conducted by Year 2 Pharmacology students Ann Marie Ming Hon, Alexia Mitcham, Adil Mohammed, Ahamad Mohammed, Inayah Mohammed, Raheema Mohammed, Saeed Mohammed, Sameer Mohammed, Tanuja Armaday, Kavya Avula, Samara Ali, Aqeela Allie, Lhonda Archer, Tariq Ali and Alviero Alvada.